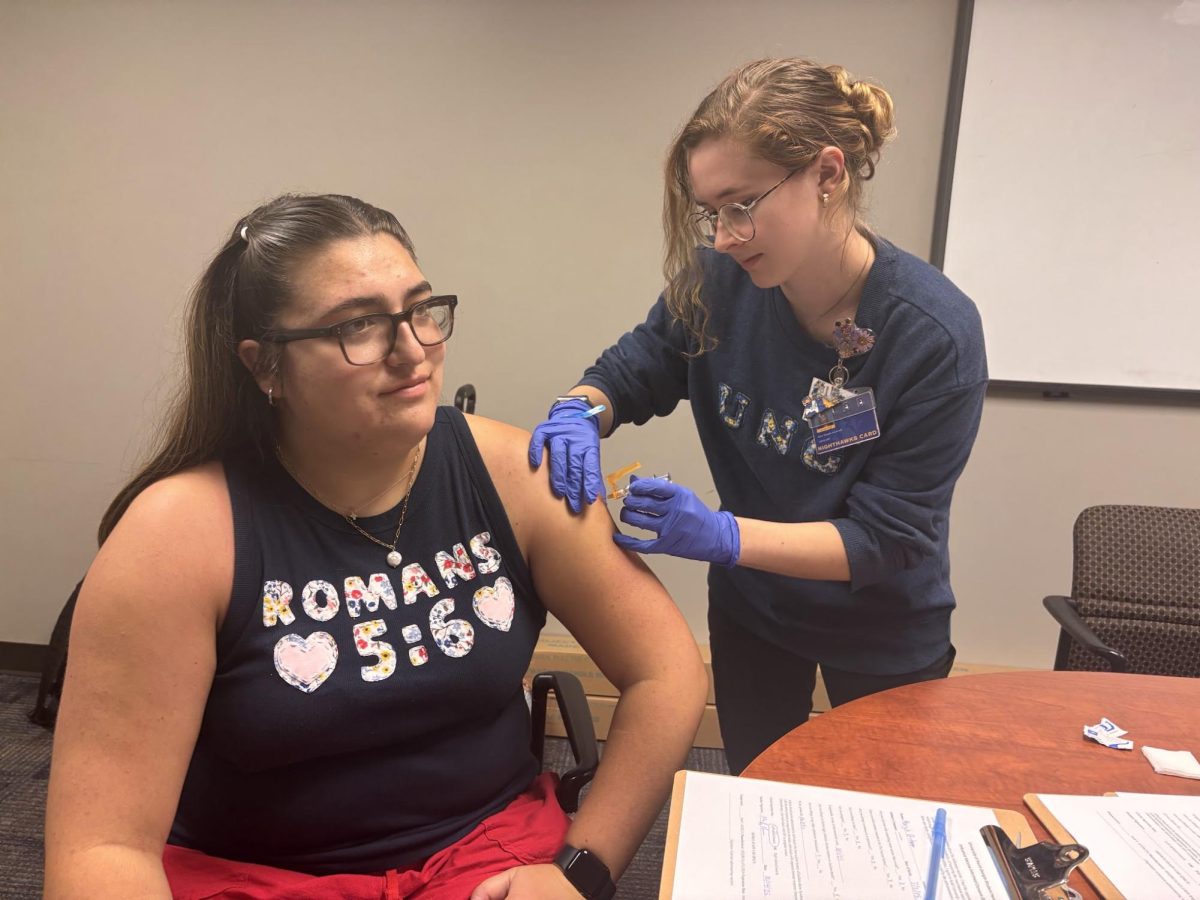
Northeast Georgia Medical Center (NGMC) has been a leading hospital in combating the fight against COVID-19.
However, with the rise of COVID-19 during the summer, NGMC has reached maximum occupancy.
Currently, 515 beds are occupied with patients, and 119 of them are in the Intensive Care Unit (ICU).
The ICU is receiving high admissions rates, causing shortages of beds, leading the ICU only to have ten beds left for emergency patients.
NGMC’s solution was to create a Medical Care Intensive Unit 2 and 3 (MICU2/MICU3). However, there is no proper ventilation in some MICU2 and MICU3 rooms, referred to as negative pressure rooms.
According to Compliant Healthcare Technologies, it is critical for hospitals to have this during COVID-19 because some individuals are more vulnerable to airborne infections.
Negative pressure rooms contain airborne contaminants within the room, and the room sucks the air in and forces it out.
Mary Bass, the Charge Nurse for MICU2, explains how they always try and make it safe for the patients.
Bass describes how she has 30 patients in MICU2, and none of them are in negatively pressurized rooms, and their only separation is a curtain. Since MICU2 does not have proper ventilation, the nurses must wear N95 masks all day.
“It is always a risk when going into a room, but for the most part [nurses] are in and out of the room so much it’s on your clothes, on your gowns it’s just everywhere,” said Bass.
Bass explains how MICU2 felt like the same working conditions of negatively pressurized rooms and that nurses go into work every day knowing the risk.
Another local ICU nurse explained how NGMC’s lack of negatively pressurized rooms makes for the feeling of an unsafe work environment, especially since they “are in a hot spot for 12 hours a day.”
The nurse also states that NGMC is severely understaffed, making it challenging to treat patients effectively. Currently, nurses can be given four patients to one nurse on any given day or night.
“It is not a safe way to staff in the ICU because a lot of these patients need detail-oriented a
nd critical thinking nurses, and they can’t do that if they are distracted with too many.”
The understaffing of nurses “creates less optimal conditions for receiving care,” said a local nurse.